Zirconia Crowns - How the Right Cement Can Minimize Failures
In 2023, the U.S. digital dentistry market is valued at $1.26 billion and projected to be valued at $1.78 billion by 2030. Concurrently, the value of...
1. Modulus of Elasticity (Elastic Modulus)
Enamel exhibits a high modulus of elasticity (~80–90 GPa¹), while dentin is significantly more flexible (18–20 GPa¹). A composite that mimics these differences—especially dentin’s flexibility—can dramatically improve the long-term performance of restorations, particularly in high-stress or deep preparations.
Clinically, this matters when restoring deep Class II or posterior lesions close to the pulp, where a stiffer-than-necessary material may concentrate stress at the margins or transmit occlusal loads directly to the underlying tooth, increasing the risk of fracture or postoperative discomfort. A dentin-like modulus allows the restoration to "give" under pressure, absorbing and distributing forces more like the natural tooth—improving the restoration’s lifespan and your patient’s comfort.
2. Compressive and Flexural Strength
While stiffness governs deformation, compressive and flexural strength govern survival. Enamel can withstand about 384 MPa² in compressive forces, and dentin around 297 MPa². Flexural strength in dentin ranges from 100–150 MPa². Leading biomimetic composites are engineered to match or exceed these numbers, with compressive strengths of 350–450 MPa and flexural strengths between 120–160 MPa.
This is particularly important when managing patients with parafunctional habits or heavy occlusion. A restoration that lacks these strength thresholds may wear prematurely or fracture under repeated loading. By selecting a material with both strength and flexibility, clinicians can confidently treat bruxers, restore function in high-load areas, and reduce the likelihood of restoration failure or retreatment. These properties also mean fewer emergencies and a smoother long-term experience for patients—something they’ll notice and appreciate.
3. Wear Resistance
Enamel’s natural wear rate is incredibly low—about 1.5 μm/year⁴—helping it maintain occlusal anatomy and function over decades. A biomimetic composite that closely replicates this characteristic is crucial for protecting the occlusal scheme and preventing accelerated wear on opposing dentition.
From a clinical standpoint, wear resistance isn’t just about how the material survives—it’s about how it maintains esthetics, function, and contact over time. A composite with poor wear resistance can flatten occlusal anatomy, disrupt the bite, and lead to food impaction or shifting contacts. Biomimetic materials maintain anatomical form, support stable occlusion, and reduce adjustments or touch-ups—benefiting both the restorative dentist and the hygienist at recalls. They also give patients restorations that feel natural, function intuitively, and don’t become a problem years down the road.
4. Coefficient of Thermal Expansion (CTE)
Enamel and dentin expand and contract at rates of roughly 11.4 ppm/°C and 8–11 ppm/°C⁶, respectively. If a restorative material deviates too far from this behavior, temperature changes from food or drink can cause microgaps, stress at the adhesive interface, or eventual marginal breakdown.
Clinically, this property is often invisible—until it becomes a problem. Patients returning with marginal staining, sensitivity, or secondary decay at the margins may be experiencing the subtle effects of thermal mismatch. By selecting a composite with a closely matched CTE, dentists can minimize these complications, preserve the bond over time, and protect the tooth-restoration interface from thermal stress. The result? Fewer callbacks, less sensitivity, and stronger, longer-lasting margins.
5. Polymerization Shrinkage and Stress
All light-cured composites undergo polymerization shrinkage—usually around 2% by volume—which creates internal stress and can pull against bonded margins. Natural tooth structure, of course, doesn’t shrink. Biomimetic composites reduce this problem by minimizing resin content and maximizing filler load—achieving shrinkage rates below 2%⁷ and dramatically reducing shrinkage stress.
This becomes clinically significant in cases with thin remaining walls, wide cavity preparations, or deep margins. High polymerization stress can cause gap formation, marginal discoloration, or even post-op pain. By choosing a low-shrinkage, nano-hybrid composite with up to 95% filler content⁸, clinicians can reduce the risk of these complications, ensure better marginal adaptation, and increase the overall integrity of the restoration. Patients will experience fewer symptoms after treatment, and the dentist will enjoy greater confidence in the bond and long-term performance.
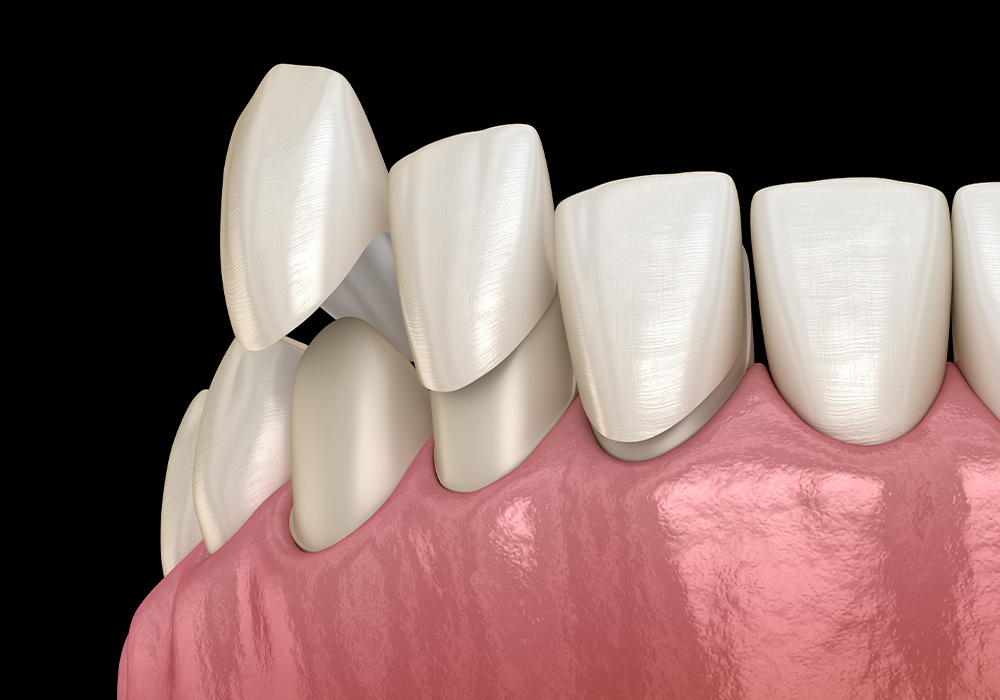
Aesthetics That Last
Beyond color and shade, truly biomimetic composites replicate translucency, fluorescence, and light refraction—enabling lifelike restorations even in challenging anterior cases. When these optical properties match natural enamel and dentin, layering becomes more efficient, margins become invisible, and results last.
Long-Term Durability
Composites that flex and resist wear like natural teeth avoid the cycle of marginal breakdown, debonding, or fracture. This is especially valuable in full-arch rehab cases, high-function posterior zones, or multi-surface restorations, where longevity is key.
Marginal Integrity and Prevention of Caries
By matching mechanical and thermal behavior, biomimetic materials reduce stress at the adhesive interface. This translates directly into fewer microleaks, reduced secondary caries risk, and better seal longevity—critical for any restorative case but especially for deep subgingival margins or high-caries-risk patients.
Improved Patient Comfort and Confidence
Composites that mimic dentin’s ability to flex and respond to temperature help minimize post-op sensitivity. This not only makes the procedure more pleasant, but reduces the need for follow-up care—leading to happier, more confident patients who trust your work.
Conclusion
A composite’s ability to “look like a tooth” is no longer enough. Today’s best materials go further—mimicking how enamel and dentin behave under pressure, over time, and across temperatures. These biomimetic properties matter not only for restoration survival, but also for reducing patient sensitivity, preventing failure, and elevating the standard of care. With the right composite, dentists can deliver restorations that look natural, feel natural, and perform like the real thing—for years to come.
1Kinney JH, Marshall SJ, Marshall GW. The mechanical properties of human dentin: a critical review and re-evaluation of the dental literature. Crit Rev Oral Biol Med. 2003;14(1):13–29.
2Habelitz S, Marshall SJ, Balooch M, Marshall GW. Nanoindentation and storage of teeth. J Biomech. 2002;35(7):995–998.
3Ilie N, Hickel R. Investigations on a methacrylate-based flowable composite based on the SDR technology. Dent Mater. 2011;27(4):348–355.
4Yap AU, Teoh SH, Hastings GW. Comparative wear ranking of dental restorative materials utilizing different wear simulation methods. J Oral Rehabil. 1998;25(2):112–118.
5Ferracane JL. Resin composite—state of the art. Dent Mater. 2011;27(1):29–38.
6Sakaguchi RL, Powers JM. Craig's Restorative Dental Materials. 13th ed. Elsevier; 2012.
7Cramer NB, Stansbury JW, Bowman CN. Recent advances and developments in composite dental restorative materials. J Dent Res. 2011;90(4):402–416.
8Ilie N, Hickel R. Resin composite restorative materials. Aust Dent J. 2011;56(s1):59–66.
In 2023, the U.S. digital dentistry market is valued at $1.26 billion and projected to be valued at $1.78 billion by 2030. Concurrently, the value of...

GrandioSO, VOCO's universal, light-cured, 89% filled nano-hybrid composite, celebrates its 10-year anniversary in 2022. Its success is a function of...